Wisdom Teeth
 Wisdom teeth (also referred to as the “third molars”) generally do not push through the gums until the late teens, twenties or sometimes even older. Wisdom teeth are usually the last teeth to erupt through the gums.
Wisdom teeth (also referred to as the “third molars”) generally do not push through the gums until the late teens, twenties or sometimes even older. Wisdom teeth are usually the last teeth to erupt through the gums.
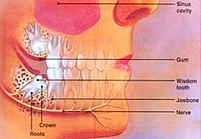
Most people have four wisdom teeth, although some people have none at all. Frequently, there is not enough space at the rear of the jaws for wisdom teeth to erupt easily through the gums. If the jaw does not allow enough room for the wisdom tooth to come through, the tooth will become crammed or “impacted”.
Some impacted wisdom teeth remain buried and cause no trouble whatsoever. However, other impacted wisdom teeth may cause severe problems.
If one or more of your wisdom teeth become problematic, your oral and maxillofacial surgeon may recommend that they be removed.
Removal of a wisdom tooth or wisdom teeth is a very common procedure. Removal of troublesome wisdom teeth should usually be performed as soon as possible so as to avoid further problems.
As shown in this illustration, an impacted wisdom tooth may be in contact, or be close to a major nerve. This can sometimes lead to complications during surgical removal of the tooth, as outlined further on.
Treatment of Potential Infection
Your dentist may be required to gently clean the infected area around the tooth. You may also be advised to rinse your mouth frequently with warm salt water mouth washes. Use one teaspoon of salt in a glass of warm water. The water should be as warm as you can safely tolerate, but not too hot.
Your surgeon may also suggest a particular mouth wash and oral pain relief.
Your surgeon may need to prescribe antibiotics. It is important to inform your surgeon if you have ever had an allergic reaction to any antibiotics or other medications. It is essential that you take the complete course of antibiotics. If a lower wisdom tooth is infected, it can be made worse by the upper wisdom tooth biting down on the gums. Removal of the upper wisdom tooth will help in this situation.
Consent Form
If you decide to undergo tooth extraction/s, your surgeon will ask you to sign a CONSENT FORM. Read it carefully and if you have any questions are concerns, ask your surgeon.
Problems Caused By Impacted Wisdom Teeth
 Infection
Infection
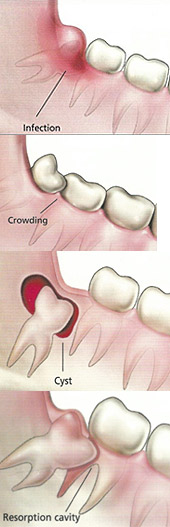
When an impacted tooth starts to push through the gum, an infection may start around the top of the tooth. Infection and inflammation can cause pain, swelling and jaw stiffness. Swallowing may also be painful. The person may feel generally unwell. The infection can also cause bad breath and an unpleasant taste in the mouth.
Crowding
A wisdom tooth may push nearby teeth out of their correct position.
Pain
Pressure from the wisdom tooth may cause pain in the tooth beside it. Pain can also be caused by infection around the wisdom tooth itself.
Cyst
If a wisdom tooth is not extracted, a sac of fluid called a “cyst” can form around the tooth and may displace the tooth. The cyst can destroy bone and damage other teeth and the gums. Cyst formation around unerupted teeth is a fairly common condition.
Ulcer
An upper wisdom tooth may push sideways out of the gum. It may cause an ulcer where it rubs against the inside of the cheek.
A food trap
Food can become lodged between the wisdom tooth and the molar next to it. This can potentially cause cavities in both teeth.
Resorption cavity
An impacted wisdom tooth may continue pushing against the molar next to it. This can cause a “resorption cavity” where the wisdom tooth hits the other molar. This often leads to serious damage to both teeth. The molars may become infected or develop abscesses. Removal of both molars is often required. Resorption cavities are uncommon.
The Decision to Remove Teeth
Following examination of your mouth, jaws and x-ray films, your surgeon will discuss the diagnosis with you. Your surgeon may recommend removal of one or more wisdom teeth, or possibly other options of treatment.
Early Removal Of Wisdom Teeth
It is generally a course of action to have troublesome wisdom teeth removed while a person in young. In young people, a tooth’s roots have not formed completely, and the bone surrounding the tooth is softer. This allows for easier removal of the tooth and there is less risk of damage to nerves, bone or other teeth.
Your surgeon may recommend early removal of one or more wisdom teeth for the following reasons:
- There is not enough space for the tooth to push through.
- You require orthodontic work and the remaining teeth must not be crowded by wisdom teeth.
- The tooth has started to become troublesome and should be removed to avoid pain, infection or other problems.
- As the molar develops a root, its involvement with a nerve of the jaw can cause postoperative complications.
- Adjacent molars need to be protected from the impacted wisdom tooth.
Your Dental and Medical History
Your surgeon will ask you about any problems you may have had with your teeth and general health. Some health problems may interfere with surgery, anaesthesia and postoperative care. This information assists your surgeon in planning the best possible treatment. Your surgeon may recommend blood tests or other health tests in the case of certain conditions such as a bleeding disorder.
Medications
To assist your surgeon, provide a list of all medications you are taking now or have been taking recently. This includes the contraceptive pill, blood thinners (such as Warfarin), and any other over-the-counter medicines such as aspirin or cough medications.
Tell your surgeon if you have ever experienced any allergic or bad reaction to antibiotics or any other medications.
Pregnancy
Inform you surgeon if you are or may be pregnant. This could affect your treatment options, including:
- x-ray examination
- anaesthesia
- pain treatment
- antibiotic drugs and other medicines
- whether removal of a wisdom tooth should be delayed.
Bleeding or Blood Disorders
Tell your surgeon if you:
- bleed too much when you are injured or have surgery
- have any blood disorders, such as haemophilia
- are taking any blood thinners such as aspirin, warfarin or Clopidogrel, among others
Smoking
It is important that you cease smoking two weeks prior to your surgery. Smoking impairs healing and increases the risk of postoperative infection.
 X-Ray Examination
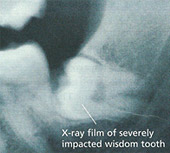
X-Ray Examination
Your surgeon will need to organise x-ray films of your jaw. The films will help your surgeon plan the best way to remove troublesome wisdom teeth.
Where to Have The Surgery
Your surgeon will advise you whether your wisdom teeth should be removed in the hospital or day-procedure clinic.
Anaesthesia
Following discussion with your surgeon, a decision will be made whether the wisdom tooth/teeth require extraction under a local or general anaesthetic. Discuss the options with your surgeon.
Local anaesthetic: If the surgery is fairly straight forward, your surgeon may suggest a local anaesthetic with a needle. The local anaesthetic will numb gums and lower parts of the face. The surgeon can then remove the tooth.
IV sedation: Some patients may benefit from a sedative drug administered into a vein during local anaesthesia to help relieve pain and anxiety.
General anaesthesia: For some people, your surgeon may recommend a general anaesthetic. General anaesthesia is administered by a specialist anaesthetist. If may be required in people who:
- have wisdom teeth that will be difficult to remove
- do not want to remain awake during the surgery
- have other problems with their wisdom teeth, gums or jaws
- need multiple teeth to be extracted
Modern anaesthesia is safe with few risks. However, a few people may have serious reactions to them. If you have ever had a reaction to an anaesthetic drug, tell your surgeon.
Removal of Wisdom Teeth
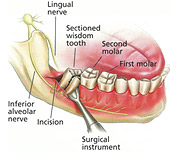 Your surgeon will make an incision to open your gums to extract the wisdom tooth. A small portion of the bone may need to be removed so your surgeon can easily get to the tooth. The tooth may have to be divided into segments so it can be removed effectively and safely.
Your surgeon will make an incision to open your gums to extract the wisdom tooth. A small portion of the bone may need to be removed so your surgeon can easily get to the tooth. The tooth may have to be divided into segments so it can be removed effectively and safely.
The incision in your gums may have to be closed with stitches. Some stitches are self-dissolving after a few days. Other stitches will be removed by your surgeon.
NOTE: For six (6) hours prior to your surgery you cannot eat or drink anything. If your surgery will be performed in the morning, you may not eat or drink anything after midnight the night before. Your surgeon will give you full instructions and written information for you to take home.
Following Surgery
Following your surgery, you will be required to rest for a while before you go home. Your surgeon will check on you as you recover. When your surgeon is satisfied with your recovery, you will be allowed to go home.
A family member or friend should take you home after the surgery. Arrange this well in advance. You are advised not to drive a motor vehicle following surgery. If you have been staying in hospital, you will return to your room when you have recovered from the anaesthetic.
Taking Care of Yourself
- Rest at home following the surgery.
- Do not drive a motor vehicle, engage in active exercise or operate machinery.
- You may need to take several days off from work, school or other duties.
- Do not consume any alcohol while you are taking pain medication or antibiotics.
Pain Relief Following Surgery
Pain may be minor in some people and greater in others. Your surgeon will prescribe pain relief for you. If you are uncertain about the best pain relief medication for you, ask your surgeon. Pain usually begins to decrease after the second day. However, some people may still need pain relief after one week. If your pain does not seem to be improving as the days go by, inform your surgeon. Further pain management may be required.
Control of Bleeding
You can apply pressure over the area of bleeding by biting gently but firmly on a piece of cotton gauze. The pressure helps to stop bleeding and a blood clot forms. It is important not to disturb the area or bleeding may start again. The gums may ooze blood slightly for a day following surgery. Any bleeding should stop by the second day. If bleeding does not stop, contact your surgeon.
Swelling
Swelling almost always occurs following surgery and can vary from minor to severe. Most swelling takes 4-5 days to settle down completely. Swelling can be reduced by applying ice packs on the cheeks.
Follow Up
You may be required to attend a follow up visit with your surgeon. Your surgeon may wish to check on healing and remove any stitches if required.
Possible Complications of the Surgery
As with all surgical procedures, wisdom teeth surgery does have potential risks, despite the highest standards of surgical practice. Whilst your surgeon endeavours to minimise any risks from your surgery, complications can sometimes occur, and occasionally some may have permanent effects.
Your surgeon will outline every possible or rare complication of your surgery. However, it is important that you have enough information to fully weigh up the benefits and risks involved with the surgery. Most people will not experience any complications, but if you have concerns about possible side effects, discuss them with your surgeon.
The following possible complications are listed to inform you and not to alarm. There may be others that are not listed.
Numbness or altered sensation
An impacted tooth may be close to major nerves (see pages…….). When the tooth is extracted, the nerve may become bruised. This can cause pain, numbness, tingling and loss of feeling in teeth, gums, cheeks, lips, chin, tongue and around the upper and lower jaw. If the lingual nerve is damaged, there is a risk of altered taste sensation. Speech may be affected in some cases.
If a nerve is injured, it will generally heal. As it heals, the numbness, tingling, pain and any dysfunction will go away. This may take four to eight weeks. In the meantime, keep hot foods and drinks away from numb areas and be careful not to bite the lip or tongue.
In some people, complete healing of the nerve may take six to eighteen months. In rare cases, the nerve may not heal completely, and numbness or altered sensation may be permanent. If feeling is reduced in the tongue, lips or face, or if speech or taste is affected, this can create major problems for some patients, particularly if it affects their daily work. If this might apply to you, tell your surgeon so these risks can be further discussed.
Nerve damage causing pain
In rare instances, an injured nerve may heal poorly and pain may persist or recur without diminishing. This can happen even though the surgery was successful and all care was taken to avoid injury to major nerves. It is now known why some nerves react in this manner. The pain in these cases can sometimes be difficult to treat.
Dry socket
Following wisdom tooth extraction, a blood clot will form over the bone. This clot is important for proper healing and relief of pain. If the blood clot is washed away or dissolves, the bone will be exposed. This is called a “dry socket”. This results in a constant, throbbing pain, that may last for several days. If you have pain like this, contact your surgeon.
- To help prevent a dry socket
- For the first day following surgery, do not rinse out your mouth or spit with force. This can loosen the blood clot and may delay healing.
- Following the first day, you can rinse your mouth very gently with warm salt water. Rinse gently every four hours or more often if required. This will assist with healing, reduce swelling and pain and reduce the risk of infection.
- Do not smoke after surgery. Smoking interferes with healing.
- Following the first day after surgery, do not brush your teeth around the area of surgery. After the first day, brush gently.
- Infection
An infection in the gum or bone is usually treated with antibiotics. It is important that you complete the full course. Tell your surgeon if you have ever had an allergic reaction to any antibiotic or other drug. - Difficulty in opening the mouth
Pain or discomfort when opening the mouth is common after removal of a wisdom tooth. This usually disappears within a few days after the swelling goes down. - Fever
The body temperature may be slightly higher after surgery. It should return to normal after 12 to 24 hours. A fever that lasts longer may be an indication of an infection or other problems. You should contact your surgeon. - Excessive bleeding (haemorrhage)
Although uncommon, haemorrhage may occur. It may be caused by too much exertion or by vomiting. It can be stopped by putting gauze over the wound and applying pressure by biting gently on the gauze for 15 minutes. If severe bleeding does not cease, you should contact your surgeon. - Lip sores
While the tooth is being removed, pressure or stretching of the lip by the surgical instruments may cause bruising or small sores. They usually heal without any problems. These lip sores are not common. - Damage to a nearby tooth or fillings
Although rare, ween a wisdom tooth is removed, the tooth or filling adjacent to it may sustain a chip or become loose. - Vomiting
Unfortunately, some people may vomit when they are recovering from the effects of the anaesthetic. - Sinus problems
The roots of the upper wisdom teeth are in close proximity to the sinuses. In some cases, a sinus may be opened when a wisdom tooth is removed. The opening will generally heal quickly without infection. However, if an infection develops or other problems arise, more treatment may be necessary. - Weak jaw
Removal of an impacted wisdom tooth can cause the jaw bone to become temporarily weaker. Although uncommon, the jaw might break at the time of surgery or during the weeks or months afterwards whilst it is still healing. Avoid contact sports for at least four weeks following surgery.
Costs of Treatment
An estimate of fees, which lists all the fees for the complete treatment, will be given to you at the time of consultation. Cost varies according to the extent of treatment and the number of teeth extracted. Additional costs may be incurred if more treatment becomes necessary. As the treatment and outcome may alter from what was initially proposed, the final account may therefore be different from the original estimate. It is always best to discuss costs prior to treatment.
Talk to Your Surgeon
This information is intended to provide a general overview. It is not a substitute for advice from your surgeon. This information does not contain all known facts about this topic. If you are not sure about the benefits and risks associated with wisdom tooth extraction, ask your surgeon.
Your oral and maxillofacial surgeon is specially trained and will be able to answer any questions or concerns you may have about your condition, surgery or anaesthesia. Your surgeon cannot guarantee that treatment will meet all of your expectations or that there are no risks involved in undergoing treatment. You may wish to seek a second opinion from another oral and maxillofacial surgeon. This information should be used only in consultation with your surgeon.