Orthognathic Surgery
Orthognathic surgery involves correct positioning of the jaws.
Orthognathic surgery literally means “straight jaws”. This type of treatment will improve a person’s ability to chew and speak. Breathing may also become easier for some people and it may be recommended as a treatment of obstructive sleep apnoea. The surgery may also improve facial appearance.
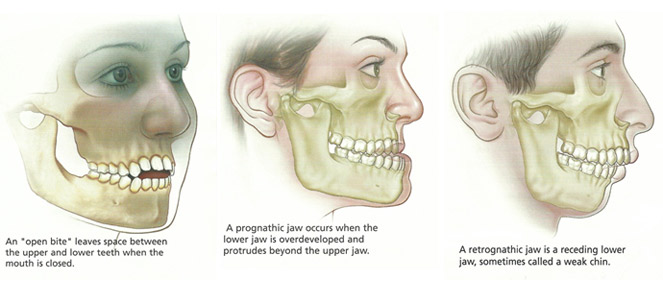
Some of the jaw problems that may be corrected by orthognathic surgery include jaws that are too large, too small, too far forward, too far back, or crooked. There may be a significant gap between the upper and lower front teeth. The causes for these problems can vary, such as:
- being present since birth
- development of the jaws as they grow
- occurring due to trauma or disease
When a person requires orthognathic surgery, it is usually performed in conjunction with orthodontic treatment to correct problems with the bite, commonly termed an “occlusion” (contact of the teeth between the upper and lower jaws as they meet during chewing or when the jaws are closed).
Symptoms and Signs
Symptoms and signs that may indicate a need for orthognathic surgery include problems with the following:
- chewing or biting food
- swallowing
- speaking clearly
- jaw pain
- unbalanced facial appearance
- facial injury or birth defects
- uneven or rapid wearing down of teeth
- open bite (space between upper and lower front teeth or back teeth when mouth is closed)
- receding chin
- protruding jaw
- Inability to make lips meet without effort
- chronic mouth breathing with dry mouth and inflamed gums
- sleep apnoea and snoring
Diagnosis
Your surgeon will examine your face and jaws and may take facial measurements, photographs or use video imaging or recommend x-ray examinations of your jaws and jaw joints. Your surgeon may assess tooth wear and tooth mobility to determine whether your teeth fit together correctly. Your surgeon may make plaster models of your teeth and jaws to assist treatment planning. You may need treatment from your general dentist before starting orthodontic and surgical treatment.
The Decision to Have Surgery
Your surgeon may recommend surgery if your jaw problem cannot be treated effectively by orthodontics alone. The recommended treatment will depend largely upon the diagnosis of your problem. Surgery is often combined with orthodontic treatment and may take from several months to two years or more to complete. You must be prepared for the overall treatment to take a long time. In some patients, psychological counselling may be an important part of the treatment.
Your surgeon will be pleased to discuss the benefits, risks and limitations of the treatment. Not treating a functional problem may:
- prevent you from being able to bite and chew your food properly, close your lips together and speak clearly
- compromise your dental health in the long term
The decision to undergo surgery is always yours. Make the decision when you are satisfied with the information you have received and believe you have been well informed of the risks and benefits.
Consent form
If you decide to undergo surgery, your surgeon will ask you to sign a consent form. Read it carefully.
If you have any further questions about the risks and benefits of the surgery, orthodontic treatment, the consent form, terms used in this pamphlet or anything else, ask your surgeon. If you are uncertain about your surgeon’s advice or diagnosis, you may wish to seek the opinion of another surgeon.
Realistic expectations
When you are making the decision to undergo surgery, it is important you bear in mind that your surgeon cannot guarantee that the surgery will always be successful or that the surgery carries no risk. The operation and its outcome might not meet your expectations.
You are encouraged to discuss at length with your surgeon the treatment and likely outcome of the surgery.
Your Medical and Dental History
Your surgeon will document your symptoms, previous treatment (if any), medical and dental history and social and lifestyle factors. Your needs to know your complete medical and dental history to help plan the best possible treatment. You will be asked to complete a detailed questionnaire.
It is important to inform your surgeon of all current and recent medications that you are taking. This includes, aspirin, cough medicines, hormone replacement therapy and the contraceptive pill. Inform your surgeon if you have ever had an allergy or adverse reaction to antibiotics, anaesthetic or any other medications.
Tell your surgeon if you are known to bleed heavily when injured or have undergone surgery, or if you have any blood disorders such as haemophilia. Surgery is usually not performed during pregnancy. Advise your surgeon if you are, could be or planning to become pregnant.
Orthodontic Treatment Prior to Surgery
 It may be necessary for some teeth to be removed prior to orthodontic treatment to facilitate space for movement of remaining teeth. The orthodontist will straighten the teeth before surgery to make the surgery simpler and to ensure a stable result. Orthodontic treatment usually lasts about 12 to 24 months, and surgery will be undertaken at some interim point. During this time you will be need to wear braces and may need to have them adjusted regularly.
It may be necessary for some teeth to be removed prior to orthodontic treatment to facilitate space for movement of remaining teeth. The orthodontist will straighten the teeth before surgery to make the surgery simpler and to ensure a stable result. Orthodontic treatment usually lasts about 12 to 24 months, and surgery will be undertaken at some interim point. During this time you will be need to wear braces and may need to have them adjusted regularly.
You may think whilst undergoing orthodontic treatment that your bite is deteriorating. However, when the surgeon moves your jaws into proper alignment (during orthognathic surgery), the teeth will be in their proper position. Orthodontics in conjunction with orthognathic surgery can optimise your outcome.
Clinical examination and records
Before your orthodontic treatment is complete, your surgeon will make final preparations for the surgical procedure. Additional records are taken. Your surgeon and orthodontist will arrange surgery when they determine that your teeth are in the correct position.
Your surgeon may use x-ray examinations and models of your teeth and jaws to decide on the surgical procedure (to be performed on your jaws) and to anticipate the results.
A plastic dental splint can be made from the model of your teeth and jaws to act as a guide for correct tooth and jaw alignment during the surgery.
Preparing for Orthognathic Surgery
Orthognathic surgery is performed in hospital under general anaesthesia. In most cases, you will be admitted to hospital on the day of your surgery. Do not eat or drink anything for fix hours prior to surgery. If your surgery is scheduled for the morning, do not eat or drink anything after midnight the night before.
If you are to undergo both upper and lower jaw surgery, you may choose to donate your own blood two to four weeks before surgery. The blood may be given back to you if there is a significant blood loss during the surgery.
Other surgical procedures
Your surgeon may recommend other procedures to maximise the outcome of the surgery, such as grafting or cosmetic procedures.
Orthognathic Surgery
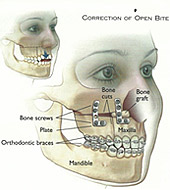
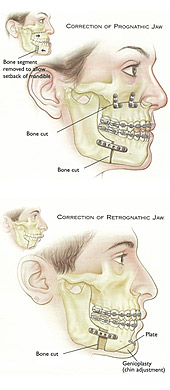 The surgeon carefully makes an incision in the bone and moves the jaw as required. For instance, a small jaw may be lengthened, or a large jaw may be reduced in size. Incisions are generally made inside the mouth so as to avoid any scarring to the face. If the surgeon needs to make an external incision, care is taken to make it in natural skin creases. Once the jaws are placed in the desired position, they are fixed permanently with small bone plates and screws. Depending upon the complexity of the surgery, this procedure may take from one hour (for a single jaw) to four hours or more (in some cases) for combined upper and lower jaw surgery.
The surgeon carefully makes an incision in the bone and moves the jaw as required. For instance, a small jaw may be lengthened, or a large jaw may be reduced in size. Incisions are generally made inside the mouth so as to avoid any scarring to the face. If the surgeon needs to make an external incision, care is taken to make it in natural skin creases. Once the jaws are placed in the desired position, they are fixed permanently with small bone plates and screws. Depending upon the complexity of the surgery, this procedure may take from one hour (for a single jaw) to four hours or more (in some cases) for combined upper and lower jaw surgery.
Hospital Stay
Your visit to hospital will usually vary from one to three nights depending upon the complexity of the surgery and your rate of recovery. You will be administered intravenous fluids and medications to prevent dehydration and infection and to minimise pain and swelling. The intravenous line and drip will remain attached to your arm after surgery until you are able to adequately take fluids and oral medications. The sooner you commence eating, drinking and moving about normally, the quicker you will be discharged from hospital.
Recovery after surgery
- Stiches: Dissolving stitches are used in most cases. These dissolve gradually over a three to four week period. If they fall out earlier, do not worry, as long as there is no ongoing bleeding.
- Jaw support: In some patients, the jaws may be held together with elastic bands during the healing phase.
- Oral hygiene and brushing: Meticulous cleanliness and care of the mouth is critical for rapid healing and prevention of infection. Brushing can prove difficult during the first week following surgery. At least four times daily you will be required to rinse your mouth with warm salt water and chlorhexidine (antiseptic) mouth wash, particularly after meal times.
- Diet: It is recommended that you consume soft foods generally four to six weeks until swelling and discomfort diminishes. Adequate nutrition is essential for healing. In the early days following surgery, eating small portions five to six times a day is recommended due to discomfort. Your surgeon will advise dietary requirements. In the latter stages of healing you may gradually return to normal eating habits. It is important however to rinse your mouth immediately following each meal.
- Work/School: It is generally advisable to take at least two weeks off work or school following your surgery. Your surgeon can issue a medical certificate to cover you for this period of absence.
- Appearance: Your appearance may have changed somewhat, so you should be prepared for the possibly of surprise from your family and friends. It will not take long for you or them to adjust.
- Orthodontist: Your surgeon will inform you when it is time to return to your orthodontist for adjustment of your bands. This is often two to three weeks following surgery. The braces will remain on your teeth for a further six to twelve months, so that your bite may be adjusted by the orthodontist to give the best possible results.
- Follow up care: Following your orthognathic surgery, you may require a further six to twelve months of orthodontic treatment to help finesse the position of your teeth and bite. Your surgeon and orthodontist will want to see you periodically to be certain that your teeth and jaws remain properly aligned. It is important to maintain good oral hygiene and visit your dentist regularly.
Possible Complications of Orthognathic Surgery
All surgical procedures are associated with some degree of risk. Despite the highest possible standards of surgical practice, complications can sometimes occur. Whilst your surgeon endeavours to minimise any potential risks or problems, complications can arise that may have permanent effects. Generally, your surgeon will not dwell at length on every possible side effect or rare complication of surgery. However, it is important to be fully informed of the benefits and risks associated with your surgical procedure. Most people undergoing orthognathic surgery will not have complications, but if you have any questions or concerns regarding possible complications, be sure to discuss these with your surgeon.
The following possible complications are intended to inform you and not to unduly alarm you.
General Risks of Surgery
- Side effects of general anaesthesia: Following a general anaesthetic, you may experience difficulty swallowing, a dry sore throat and generalised muscle pain. These symptoms generally resolve by the following day. You may experience nausea and vomiting after waking from a general anaesthetic and for one to two days afterwards. If necessary, you will be prescribed a medication to help settle the vomiting. Although rare, the risks of general anaesthesia can include bronchitis, pneumonia, a hoarse voice, heart attack, stroke and death. Elderly patients and patients with existing heart disease may be at a greater risk of heart attack.
- Infection: All surgery carries the risk of infection, particularly in patients with diabetes. The risk is low following orthognathic surgery, although infection may develop around plates and screws. Antibiotics are usually prescribed at the time of surgery to prevent the risk of infection. If infection does occur, the symptoms generally appear at 10 to 14 days following surgery with increased pain, swelling and a bad tasting discharge in the mouth. If infection or bleeding does occur, contact your surgeon immediately. In rare instances, the oral incision may require to be re-opened, cleaned and re-stitched.
- Scarring: The majority of incisions in the mouth heal well and quickly. In some people however, healing may be progress slowly, usually because they are elderly.
- Inflammation of veins: Veins that are used for intravenous fluids and medications may become inflamed, with swelling, discolouration and restriction of arm or hand movement for some time.
Specific Risks of Orthognathic Surgery
- Pain and discomfort: Pain and discomfort depend upon the complexity and difficulty of the surgery. The discomfort is generally worse during the first 2-3 days following surgery and should then gradually subside. Strong pain medication will be provided. As the discomfort decreases the need for analgesics will generally cease about 7-10 days after surgery.
- Bleeding: If too much bleeding occurs during surgery, a transfusion may be required. Bleeding may also occur in the first 24 to 48 hours following surgery, particularly if you continue to spit, smoke, touch the wounds with your fingers, or consume hot foot. To minimise the risk of bleeding, sleep with your head elevated on pillows. It is important to avoid smoking and not to rinse your mouth vigorously until the day following surgery and to get adequate rest. Bleeding may also occur if the healing wound becomes infected.
- Swelling: Swelling is to be expected following surgery. Maximum swelling occurs 48 hours following surgery and gradually subsides over three to four weeks. Most swelling subsides after the first 14 days. The more complex and difficult the surgery, the greater the swelling. You may also experience difficulty closing your molars together for a few days as a result of swelling.
- Bruising: Bruising of the face, neck and chest may occur in some people as the swelling subsides. It generally disappears in seven to ten days.
- Nerve damage: When nerve damage occurs, feeling (sensation) is impaired because nerves are moved and may be stretched during surgery. The chin, lower lip, upper lip, cheeks and palate are the most commonly affected. Older patients (over 40 years) undergoing certain types of surgery of the lower jaw are at greater risk of permanent numbness and loss of sensation. In most patients, sensation returns to normal within three to six months. Tingling and itching is a positive indication that feeling is returning. It is important to avoid biting your lips or placing hot food or drink near the numb areas until sensation has returned completely. Following upper jaw surgery, your sense of smell may be diminished for a while.
- Nasal sinus: Following upper jaw surgery, the nasal sinus will be affected for several weeks. In rare cases the patient may require further surgery to treat persistent and ongoing problems.
- Limited facial movement: Restricted mouth opening, caused by swelling and later by general jaw stiffness is normal after major jaw surgery. Elastic bands are placed between the teeth to support the lower jaw and guide the teeth into a proper occlusion (bite) after the surgery. Jaw function will gradually improve. Mouth opening returns to normal during the four to six weeks after surgery. While the jaws are secured into a rigid position, the muscles used in facial expression may not function properly because of general facial swelling.
- Loose bone screws: Generally, bone screws do not come loose. If this does occur, the problem is treated by removing the screws after the bone has healed. Patients may require further surgery to remove wires, pins, screws, plates or splints.
- Wound separation: This is a rare complication. Generally, poor oral hygiene may be the cause of wound opening.
- Delayed healing or non-healing of bone: In some patients, the bone can heal very slowly or not at all. Delayed union or non-union of the jaw bone after surgery is rare in healthy patients. Smoking increases this risk. The jaw bone may fail to heal where there is little or no bone contact between the areas where the bone has been cut. Further surgery may be needed if the bone heals too slowly. Such problems are usually overcome with bone grafting.
- Relapse: Relapse of the new jaw position or unexpected shifting of the jaw structures is uncommon, but can occur. If the jaw does not remain in its new position, further surgery is usually required. The risk of relapse is highest when the jaw is moved a greater distance. Prevention of a relapse may require bone grafts to provide a more stable result.
- Loss of teeth: Rarely, the blood supply to teeth may be affected and teeth near the bone, cut between or near the roots of teeth and on occasions root canal treatment may be required.
- Jaw joint pain: The temporomandibular joint (TMJ) is the jaw joint that you can feel nearby the ears when you move your jaws. TMJ pain or abnormal function can arise following orthognathic surgery. Surgery may aggravate existing jaw joint problems and may warrant further treatment. If you are prone to jaw pain problems please advise your surgeon.
- Velopharyngeal incompetence: This occurs when the soft palate (velum) and throat (pharynx) do not seal the space connecting the mouth and nose during speech. The problem may occur after some types of upper jaw surgery in cleft palate patients. The effect is to make speech sound more nasal than it was prior to surgery.
Report to Your Surgeon
Inform you surgeon immediately if you develop any of the following symptoms:
- Temperature higher than 38°C or chills
- Severe pain, redness or swelling of the operation site
- Nausea or vomiting
- Persistent bleeding
- Any concerns you have regarding your surgery
Cost of Treatment
Your surgeon’s rooms will advise you regarding fees and out-of-pocket expenses involved with your surgery. You will be given an estimate of fees which will list the likely costs involved in your surgery.