Pain and discomfort
Pain and discomfort depend upon the complexity and difficulty of the surgery. The discomfort is generally worse during the first 2-3 days following surgery and should then gradually subside. Strong pain medication will be provided. As the discomfort decreases the need for analgesics will generally cease about 7-10 days after surgery.
Bleeding
If too much bleeding occurs during surgery, a transfusion may be required. Bleeding may also occur in the first 24 to 48 hours following surgery, particularly if you continue to spit, smoke, touch the wounds with your fingers, or consume hot foot. To minimise the risk of bleeding, sleep with your head elevated on pillows. It is important to avoid smoking and not to rinse your mouth vigorously until the day following surgery and to get adequate rest. Bleeding may also occur if the healing wound becomes infected.
Swelling
Swelling is to be expected following surgery. Maximum swelling occurs 48 hours following surgery and gradually subsides over three to four weeks. Most swelling subsides after the first 14 days. The more complex and difficult the surgery, the greater the swelling. You may also experience difficulty closing your molars together for a few days as a result of swelling.
Bruising
Bruising of the face, neck and chest may occur in some people as the swelling subsides. It generally disappears in seven to ten days.
Nerve damage
When nerve damage occurs, feeling (sensation) is impaired because nerves are moved and may be stretched during surgery. The chin, lower lip, upper lip, cheeks and palate are the most commonly affected. Older patients (over 40 years) undergoing certain types of surgery of the lower jaw are at greater risk of permanent numbness and loss of sensation. In most patients, sensation returns to normal within three to six months. Tingling and itching is a positive indication that feeling is returning. It is important to avoid biting your lips or placing hot food or drink near the numb areas until sensation has returned completely. Following upper jaw surgery, your sense of smell may be diminished for a while.
Nasal sinus
Following upper jaw surgery, the nasal sinus will be affected for several weeks. In rare cases the patient may require further surgery to treat persistent and ongoing problems.
Limited facial movement
Restricted mouth opening, caused by swelling and later by general jaw stiffness is normal after major jaw surgery. Elastic bands are placed between the teeth to support the lower jaw and guide the teeth into a proper occlusion (bite) after the surgery. Jaw function will gradually improve. Mouth opening returns to normal during the four to six weeks after surgery. While the jaws are secured into a rigid position, the muscles used in facial expression may not function properly because of general facial swelling.
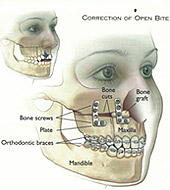
Loose bone screws
Generally, bone screws do not come loose. If this does occur, the problem is treated by removing the screws after the bone has healed. Patients may require further surgery to remove wires, pins, screws, plates or splints.
Wound separation
This is a rare complication. Generally, poor oral hygiene may be the cause of wound opening.
Delayed healing or non-healing of bone
In some patients, the bone can heal very slowly or not at all. Delayed union or non-union of the jaw bone after surgery is rare in healthy patients. Smoking increases this risk. The jaw bone may fail to heal where there is little or no bone contact between the areas where the bone has been cut. Further surgery may be needed if the bone heals too slowly. Such problems are usually overcome with bone grafting.
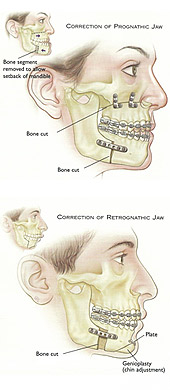
Relapse
Relapse of the new jaw position or unexpected shifting of the jaw structures is uncommon, but can occur. If the jaw does not remain in its new position, further surgery is usually required. The risk of relapse is highest when the jaw is moved a greater distance. Prevention of a relapse may require bone grafts to provide a more stable result.
Loss of teeth
Rarely, the blood supply to teeth may be affected and teeth near the bone, cut between or near the roots of teeth and on occasions root canal treatment may be required.
Jaw joint pain
The temporomandibular joint (TMJ) is the jaw joint that you can feel nearby the ears when you move your jaws. TMJ pain or abnormal function can arise following orthognathic surgery. Surgery may aggravate existing jaw joint problems and may warrant further treatment. If you are prone to jaw pain problems please advise your surgeon.
Velopharyngeal incompetence
This occurs when the soft palate (velum) and throat (pharynx) do not seal the space connecting the mouth and nose during speech. The problem may occur after some types of upper jaw surgery in cleft palate patients. The effect is to make speech sound more nasal than it was prior to surgery.